In cancer conversations, comments intended to express empathy or comfort can backfire when they are dismissive of the person’s situation, choices, decisions, or emotions. We designed our Talking Tips to help supporters avoid these pitfalls. Our Talking Tips compare unhelpful comments that, believe it or not, have actually been said to a someone with cancer with an improved and more mindful way of phrasing the sentiment.
“I’ll be here to support you.”
Talking to a friend with a life-threatening illness can be intimidating, stressful, and even awkward. It is often hard to find the right words to say, but remember, your friend feels just as unsure as you about what to do or say.
One thing that is unhelpful is making promises you can’t keep. Instead, start by letting your friend know you will be there for them, and then you can figure out what’s next…together. They need you to b-present now more than ever.
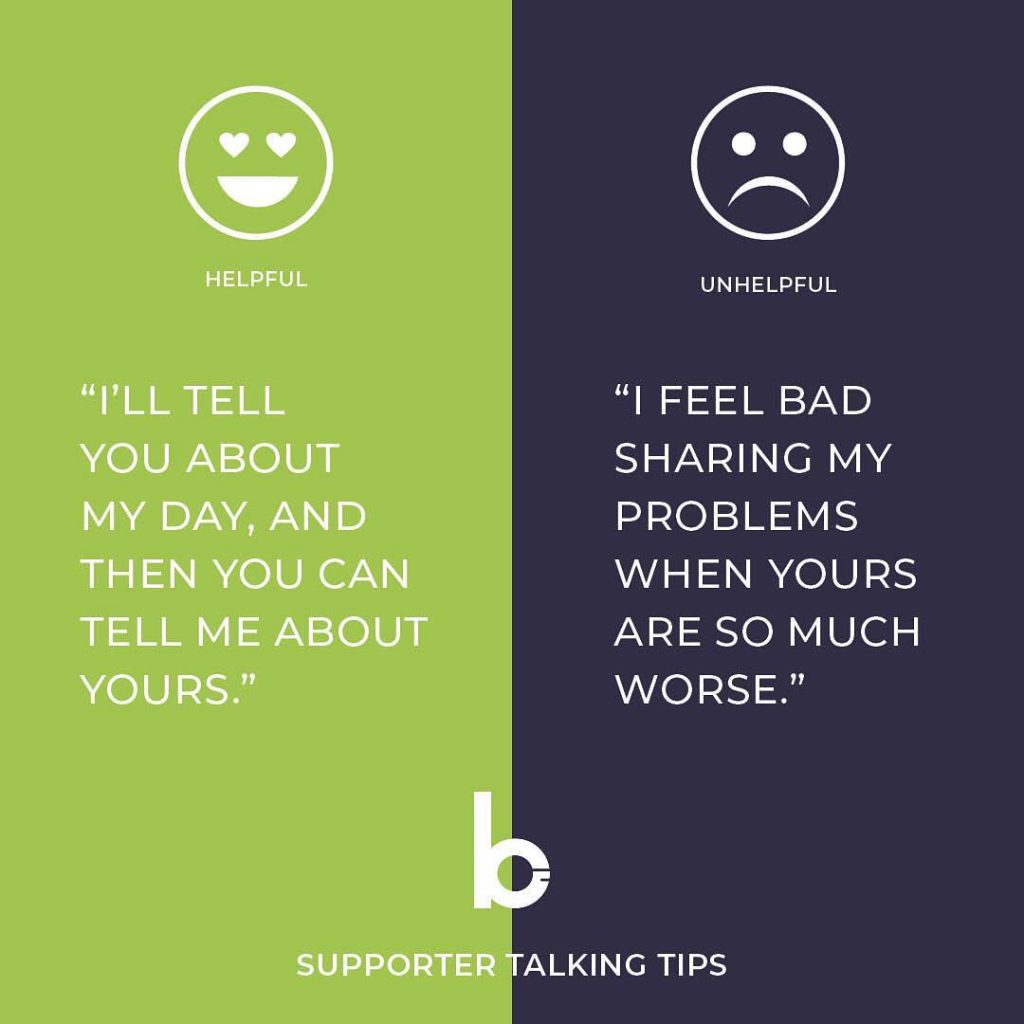
“I’ll tell you about my day, and then you can tell me about yours.”
Everyone has their struggles. Holding back information because you think it’s not worthy can make the conversation feel abnormal and frustrate the other person. They just want to have regular chats like you did before they were diagnosed. Just b-yourself, don’t be afraid to use humor, and when it comes to steering the conversation, let them be your guide!
“I am going to the store. What can I get you?”
A lot is going on the first few weeks after the diagnosis. Even though it may seem helpful to say something like, “Let me know if you need anything” to the patient or caregiver, it isn’t. It puts the burden on them and gives them another task they need to perform before they can receive help.
Instead, offer tangible things on your own and follow through. For example, offer to set up a meal train, provide rides, do laundry, get groceries, sit with the patient while the primary caregiver takes a break, etc.
Remember, it is humbling to ask for help and is sometimes hard to know what to ask for at the beginning, which can often lead to added stress, so try not to be too pushy. There may be some resistance to accept help at first (the “I don’t want to impose” feeling). Give the patient room to say no, but reinforce that it is no trouble and you are happy to help. As they get more comfortable asking for and accepting help, it will be easier as a supporter to pitch in where needed.
“I can’t imagine what you are feeling. How can I help?”
Expressing empathy by sharing stories about someone you knew who had cancer and passed away or had severe complications is not helpful. Knowing someone else’s cancer experience doesn’t mean you know what your friend is going through. Negative stories are upsetting, and often cause the cancer patient to expect the worst instead of being hopeful. So what do you say?
It’s okay to admit you have no idea what your friend is going through, so start there. Then ask how you can help them get through this. If they don’t know, then just listen. If they are looking for inspiration, help them find it. If they have questions, write them down so they can ask the doctor later. If there are important questions or resources you think might be helpful, share those when the time feels right. Help comes in many forms. Work with them to find positive and meaningful ways that get them through the day.
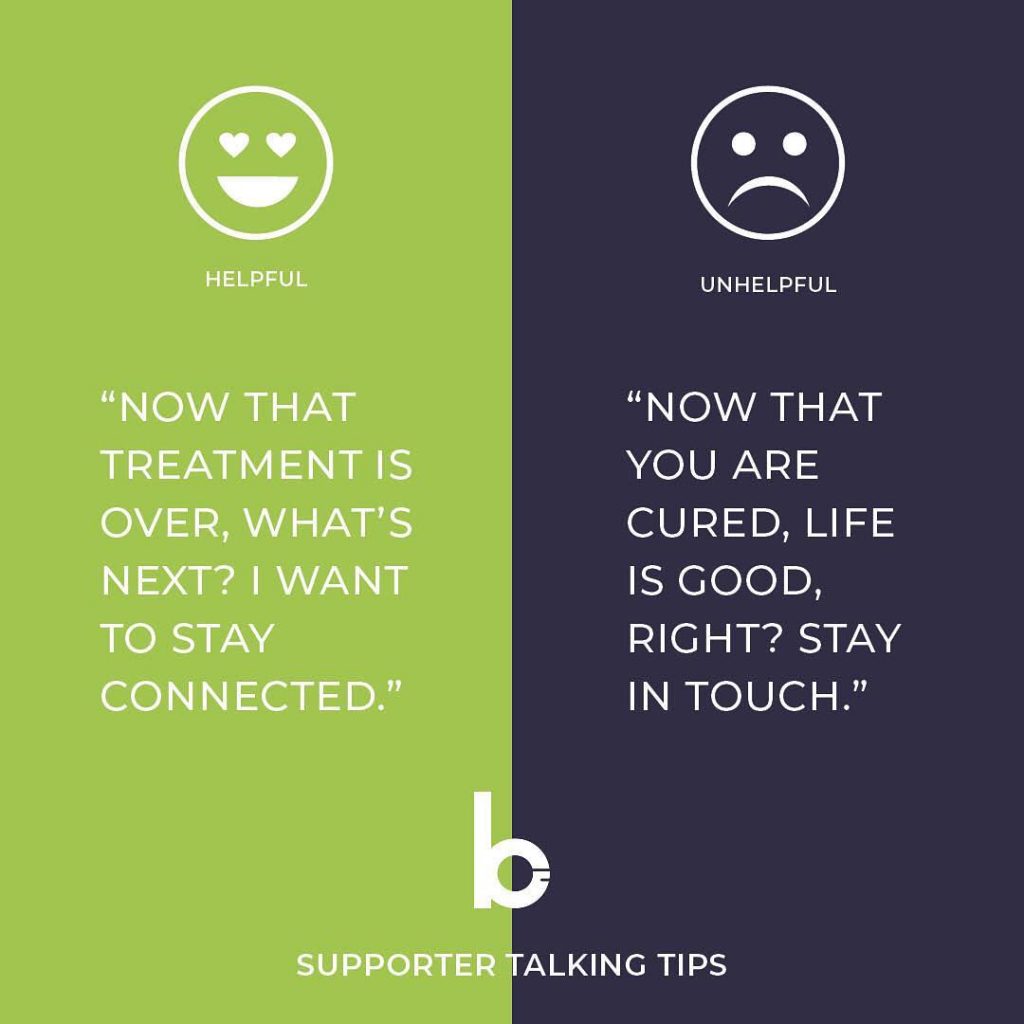
“Now that treatment is over, what’s next? I want to stay connected.”
Just because their treatment is over, doesn’t necessarily mean they are “cured.” Every cancer is different, but cancer survivors will still be in a maintenance period that could last months or years. After treatment, survivors AND supporters will be re-adjusting in different ways. There will be a sense of relief and a desire to get life back to “normal,” but there will also be anxiety and post-traumatic stress. This transition can feel even more lonely, so remember to continue to be there for each other. Offer to meet for coffee, go for a walk together, or watch the sunset.
Being a good supporter means being present and staying connected through good and bad times. If you are finding it hard to make time, add an event to your calendar that reminds you to reach out. It will mean so much!
“Yes, you look different, but it does not change who I see.”
No, it’s not just hair. It is a part of one’s identity. It is a way to express ourselves. Most of us have the freedom to style our hair to look the way we want it to look, and when you all of a sudden have that freedom taken away from you, it can be devastating and make one feel vulnerable, insecure, and uncomfortable.
Cancer patients are already going through the most challenging time in their lives, and hair loss adds to their concerns about being treated differently. When you see your friend without hair for the first time, it will be emotional, but try to match their emotions. If they cry, it’s okay to cry with them. If it seems like they want a regular hangout, hug them, sit back, and follow their lead. Remind them with your words and actions that even though they have lost their hair, it has not changed how you see them.
Avoid comments like, “It will grow back.” While it might seem like these words are encouraging, it can make your friend feel like you are disregarding their emotions. Remember, they are constantly reminded of their illness every time they look in the mirror, and yes, even though hair can grow back, it could take years.
Also, b-aware of your friend’s personal space and comfort level. Initially, they may not want visitors until they have gotten used to their new look, but you can still call or text them and give them a chance to talk about how they are feeling. Once they are ready for visitors, they may prefer to wear a hat or wig when they are around others, so make sure not to drop in unexpectedly. Give them the time to prepare so they are comfortable.
Whether it is giving them space, going with them to buy a hat or wig, connecting with them online, or simply just listening to them, the best thing you can do is b-there for them in ways that feel right at that moment. As long as you are there for them, no matter if that’s in person or online, they will always appreciate your unconditional support.
“I’ll be here to help you through this.”
Have you ever found yourself in a painful or confusing situation with a friend, and in your struggle to find the right words to say, you settle for “everything happens for a reason”? And…that’s where the conversation probably ended because, well, what could one say in response to that?
Instead of engaging in a potentially helpful and supportive conversation, we can unintentionally shut it down…covering up their pain with a blanket statement because we feel uneasy. If you want to be the best supporter you can be, learn to sit with your friend in their pain. Don’t let your discomfort get in the way of your ability to b-present for them. Assure them that you will always be a part of their support squad, through the good times and the bad.
“I see you are wearing a mask. What activity would be best today?
Have you ever seen someone wearing a mask, and thought to yourself, “I wonder what they have that could make me sick?” or “I’ll wait for the next elevator, I don’t want to be close enough to get whatever they have.” Yes, these situations have happened, and it can be very upsetting for a cancer patient that already feels different and isolated.
We often associate someone wearing a mask with a contagious disease, but did you know that when cancer patients wear masks, it is not to protect you from them, it is to protect them from their surroundings. Cancer is NOT contagious, so avoid treating someone with cancer like they have an infectious disease. Cancer patients undergoing treatment or recovering from treatment will often have compromised immune systems. This means they are more vulnerable to having severe reactions to common illnesses because their immune system is not strong enough to fight. For them having a fever doesn’t just mean taking aspirin to reduce the symptoms, it means a trip to the emergency room to avoid a life-threatening situation. Wearing a mask is part of their defense in public places.
So what should you do? When you see them with a mask, look past the mask, but don’t ignore what it might mean. Don’t make a big deal about it. Instead, follow their lead. When out in public, ask if there are any limits to activities or places they can go. Don’t make them feel bad for being cautious. Germs are their enemy, and they need to be careful, but they still want to do normal activities so help them find an option that works. Also, if you know you have a cold or are just getting over the flu, let them know, and it may be best to reschedule for another day, especially if they are in the hospital.
Being a good supporter means understanding your friend’s situation and not making them feel bad about the things that they have to do or wear for their own health and safety. This includes looking past the mask and seeing them as the incredible person they are and respecting their limits. Remember, the only thing wrong with them wearing a mask is you can’t see their beautiful smile!
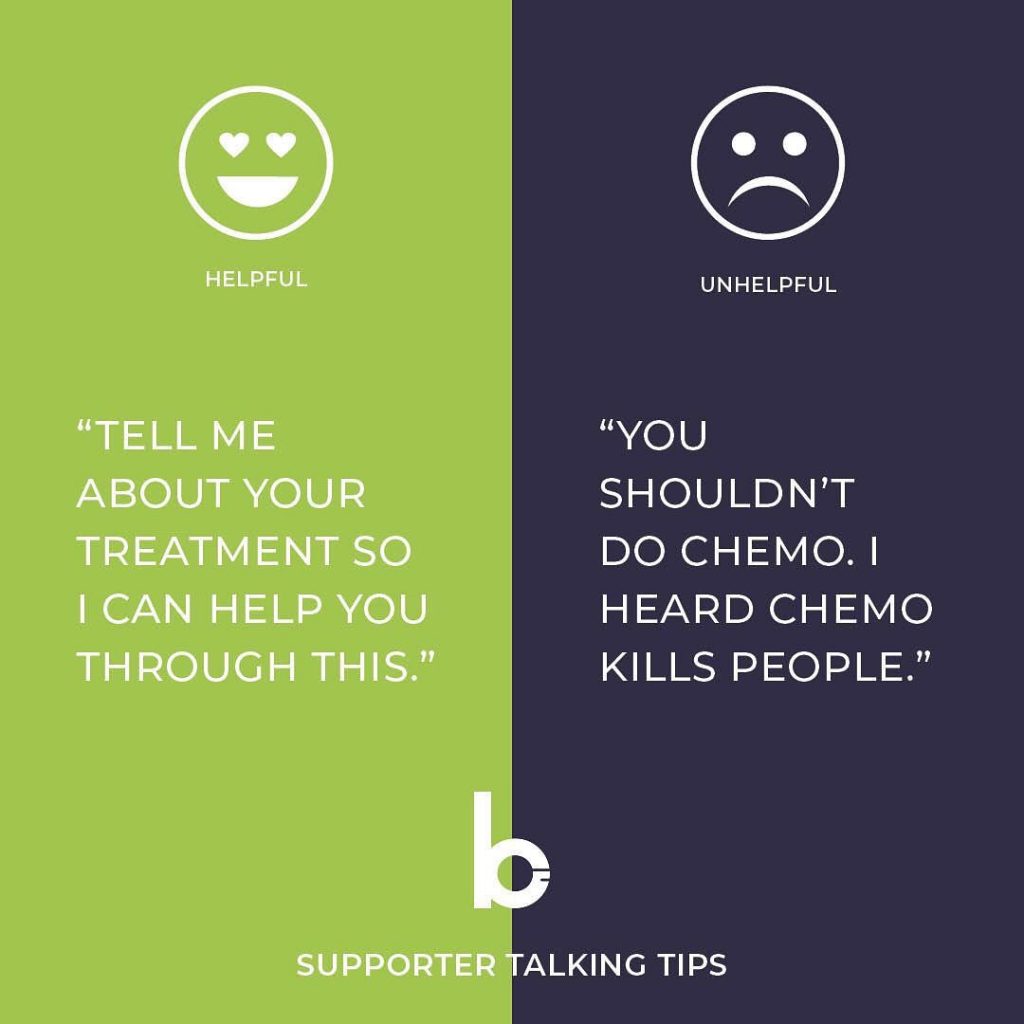
“Tell me about your treatment so I can help you through this.”
Cancer patients are fighting for their lives. Do you think they really want to do chemotherapy or radiation or take the long list of pills to manage the side effects? No way. Cancer treatments are complicated, and every patient’s treatment will be different depending on the type of cancer they have as well as their own health and history. They have consulted their doctor and other specialists and made their decision.
Unless they ask for your input, it is not helpful to judge them for their choices, make general upsetting statements about treatment, or suggest alternatives that could impact their life. Imposing your beliefs and opinions will only place doubt and worry in their mind, and lead to frustration that you are not supporting them. So what should you do?
Listen first. If they want to talk about their treatment, take the opportunity to learn more about what it is, how long it will last, and what they will be going through during each phase. Then find ways to be supportive. If they have questions about the treatment, write them down, so they remember to ask the doctors later. Ask how you can help make them comfortable or reduce their stress during their difficult treatments. Determine if there is a favorite item or activity that will take their mind off the side effects. There might be an errand or chore that they can’t do that is causing stress, so offer to do it for them. Sometimes just hanging out with them will reduce the stress, knowing they are not alone during an uncertain time.
Every day will be different. The more you understand about what they will be going through and how they feel about it, the better prepared you will be to support them in meaningful ways that bring comfort and reduce stress.
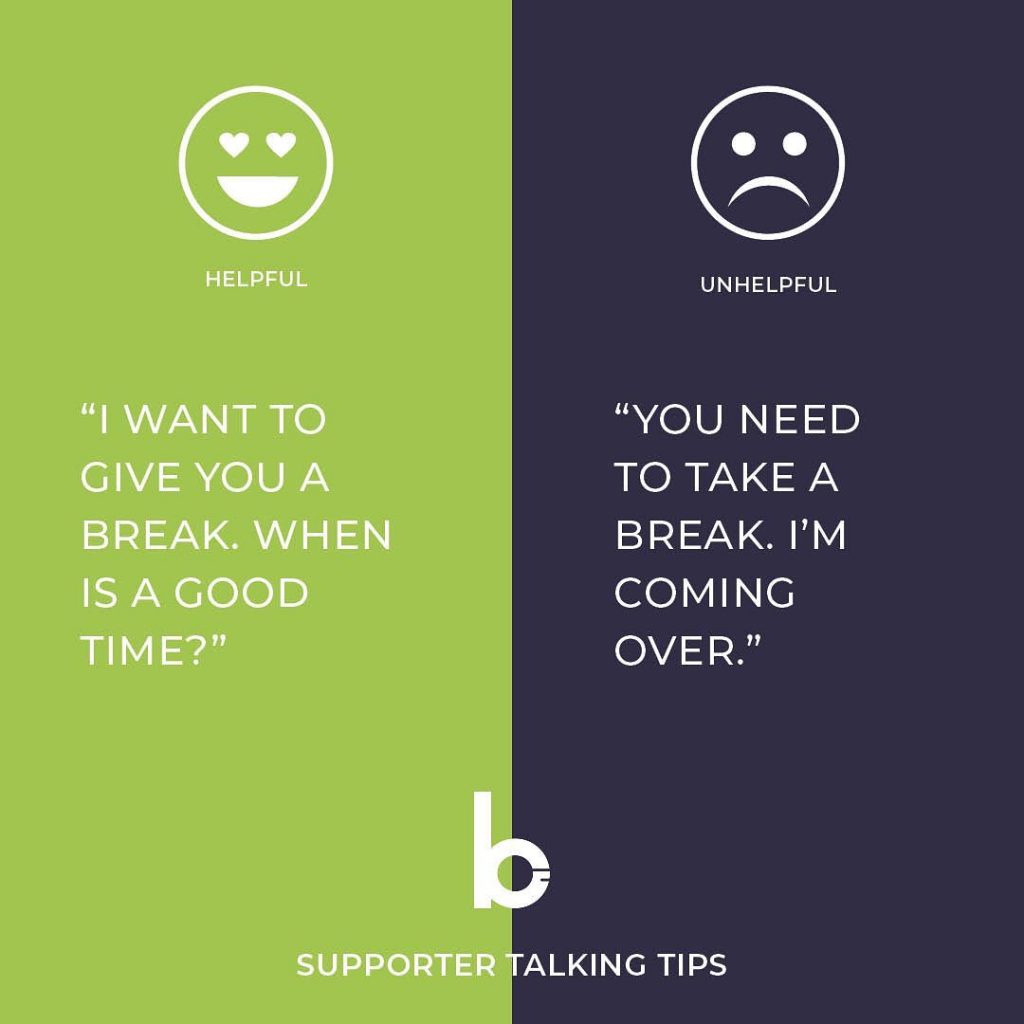
“I want to give you a break. When is a good time?”
A reminder that the primary caregiver needs our support too. They are not only experiencing high levels of stress and anxiety about the future health of their loved one, but also the future of their family unit. The primary caregiver has to be a patient advocate for an illness they knew nothing about before diagnosis and providing care and comfort in the face of unknown challenges. They can become isolated and feel they have no one to talk to for encouragement, answers, or just let off some steam. This adds to the daily stress of keeping the house and finances in order, going to work or school, and caring for the rest of the family, including pets.
Being supportive of the primary #caregiver is important to their health and well-being, so find things that will give them a physical or emotional break. It can come in many forms, like…
– Running errands
– Helping with household chores
– Bringing meals
– Bringing requested entertainment for a welcome lift
– Staying with the patient while the caregiver takes some needed “me” time
And most importantly, just listening. Give the caregiver a chance to talk and process their feelings. Whatever support you offer, ensure it reduces stress. Remember, directing help or entertaining visitors can sometimes be stressful and don’t take it personally if they decline. Agree to a fixed amount of time, so they can plan other activities, and be sure to re-confirm on the day of the event since issues will come up at the very last minute.
Be flexible with your visit, and wrap it up if it looks like they are ready for some space. Being present for the caregiver, and being mindful of their emotional and physical state when we offer support will ensure the best and most positive impact for them. It will give them the boost they need so they can continue to b-present in the best way possible for loved ones.
p.s. Don’t forget to acknowledge the primary caregiver’s sacrifices. They have given so much of themselves to bring comfort to our loved ones, and they need to hear out loud that those sacrifices are noticed and appreciated.
“I’m so glad I get to hang out with you today!”
If your friend is dealing with a life-threatening illness, saying “I feel so sorry for you” through your words and body language is unhelpful and discouraging. Ditch the pity party and figure out how to bring normalcy back into their life. Find an activity you used to enjoy together and know will give them a lift. Often the actions and words that are most appreciated are the ones that make them feel more like a person less like a patient.
“You are not alone. It is okay to be feeling what you are feeling.”
We all go through tough times, and people help us through them. When chatting with a friend who is struggling with their mental health, it is crucial to provide a non-judgemental space where they can be open about how they are feeling.
A few tips:
- Don’t second guess their feelings. While you may be happy to chat and offer support, chances are you aren’t a trained counselor. Try not to make assumptions about what is wrong or jump n too quickly with your own diagnosis or solutions.
- Let them lead the conversation and don’t pressure them to tell you anything they aren’t ready to talk about. Talking about their struggles with someone else takes courage and trust.
- Listen with no distractions. Your friend wants to feel heard. Repeating what they said back to them ensures them that you understood and lets them know that you respect their feelings.
- Keep questions open-ended. Try to keep your language neutral. Give the person time to think about and answer your questions, but try not to bombard them with too many questions.
- Offer to help them find professional support. You can offer to the doctor with them or help them talk to another friend or family member. But try not to take control and allow them to make decisions.
Want more?